Q. How to find the right doctor for my anal fistula treatment? How to ensure that I don’t get operated by a quack?
Anal fistula treatment is available throughout the country. Till some time back, anal fistula and hemorrhoids (piles) were mostly taken care of by quacks. The main confusion occurs because these quacks do massive, lucrative advertising, give assurance of a 100% cure rate, have fewer charges, and assure of minimal side effects or harm. Due to this, many people fall prey and get treated by these quacks. These unqualified and under-experienced self-styled “piles experts” show testimonials of treated patients to convince patients of their clinical experience. All this causes a lot of confusion in the mind of a layperson. In this regard, there are a few crucial points worth understanding:
- Any medicine or treatment procedure that has a positive effect on the body can also potentially harm the body. Only a medicine that has NO effect at all can be assured to have no negative impact on the body. Because, logically, if the medicine is going inside the body and changing some tissues or organs to bring positive effects, that medicine can always have some negative effects too. Most treatments used in allopathy, homeopathy, Ayurveda, etc., have more beneficial effects than negative side effects due to which these medicines have been in use for so many years. If some system claims that there are no side effects, then, at most, we can say that the negative side effects have not been studied or documented or are unknown. So, the claim by quacks that their medicines or procedure will have no side-effect cannot be valid.
- The testimonials,which include videos of successfully treated patients, are also used to misguide laypeople. These testimonials should be analyzed carefully. It is essential to understand that fistulas are basically of two types – simple or complex. About two-thirds of anal fistulas are simple, and one-third of fistulas are complex. The simple fistulas, as the name suggests, are simple to treat. Most of these fistulas will get alright irrespective of the procedure done. So, treating a simple fistula does not necessarily convey the surgeon’s expertise. Any procedure such as cutting surgery, ksharsutra, cutting seton (thread), VAAFT (doorbin), laser, plug, or flap will cure most simple fistulas without any risk to the patient.
On the other hand, complex fistulas, as the name suggests, are complicated and should be handled very carefully. Complex fistulas are the recurrent fistulas (which tend to occur again after an operation has been done) or high fistulas involving more than one-third (33%) of the sphincter muscle (the muscle which controls the bowel motions). High fistulas are considered complex because most procedures are done by routine surgeons or quacks like fistulotomy, cutting seton, Ksharsutra, etc. will damage the sphincter muscle and thus can cause incontinence (losing control over bowel motions- the person will not be able to control stools). Therefore, complex fistulas should always be treated by an expert fistula surgeon in the region, preferably in the country, as the stakes are very high.
Main risks of complex anal fistula
Incontinence: As discussed above, the risk of losing control of motions (stools) is very high if complex fistulas are treated by routine surgeons or quacks
Recurrence: The chances of fistula not getting cured or occurring again are also very high (50-80%) if complex fistulas are treated by someone who is not a renowned fistula expert
So, the quacks show the testimonials of simple fistulas treated by them to convince people of their expertise. The laypersons do not know the difference between simple and complex fistulas and think that all fistulas are the same. They get impressed by testimonials of a patient with a simple fistula having been treated by a quack. So, it is important that we should not be impressed by any testimonial but should try to look for an experienced surgeon who has done original work in the field of anal fistulas.
Secondly, it is essential for us to know whether our fistula is simple or complex.
Q. How to know whether my fistula is simple or complex?
You can know that your fistula is complex if you have either of these three.
- Recurrent fistulas: If your fistula occurs again after the first surgery, then your fistula is complex. This is so because most simple fistulas get cured after the first operation.
- High fistula: If your fistula involves more than one-third (33%) of the sphincter muscle (the muscle that controls the bowel motions), it is a complex fistula. This is so because the risk of damage to the sphincter muscle is high while operating these fistulas.
- Garg classification grade III, IV, or V:Garg classification has been innovated by Dr. Pankaj Garg and is being used by surgeons and radiologists worldwide.1-4This is known as the Garg classification of anal fistulas. As per Garg classification, grade I & II fistulas are simple fistulas and grade III, IV & V fistulas are complex fistulas. So, grade III, IV & V fistulas should only be treated by an experienced well, qualified fistula surgeon.
So, Recurrent fistulas, High fistulas and Garg grade III, IV & V fistulas are complex fistulas.
References
- Garg P. Garg Classification for Anal Fistulas: Is It Better than Existing Classifications?—a Review. Indian Journal of Surgery 2018; 80(6): 606-608 ( Click here for DOI )
- Dawka S, Yagnik VD. Comparison Between the Modified Parks and Garg Classifications of Cryptoglandular Anal Fistulas. Dis Colon Rectum 2021 ( Click here for PubMed , Click here for DOI )
- Garg P. Assessing validity of existing fistula-in-ano classifications in a cohort of 848 operated and MRI-assessed anal fistula patients – Cohort study. Ann Med Surg (Lond) 2020; 59: 122-126 ( Click here for PubMed, Click here for DOI )
- Garg P. Comparing existing classifications of fistula-in-ano in 440 operated patients: Is it time for a new classification? A Retrospective Cohort Study. Int J Surg 2017; 42: 34-40 ( Click here for PubMed, Click here for DOI )
Q. What are the risks of a complex fistula?
The main risk of a complex fistula is that if treated by a routine surgeon or a quack, then the risk of recurrence (fistula occurring again) or incontinence (losing control over bowel motions) is very high. Moreover, after each recurrence, the fistula becomes more and more complex and challenging to treat.
Q. What if I do not treat my anal fistula?
If the anal fistula is not treated timely, then there are chances that the fistula might become more complicated with time. Second, an acute abscess can form in the fistula at any time, which would create an emergency. Third, after a few years, the risk of cancer also becomes more.
Q. What should I do if I have a complex fistula?
First, get it confirmed that you have a complex fistula. The three criteria that make a fistula complex have been listed before (Recurrent fistulas, High fistulas, and Garg grade 3,4 & 5 fistulas).
Once it’s confirmed that your fistula is complex, then it is imperative that you search for a fistula expert surgeon.
Dr.Pankaj Garg is a world-renowned fistula surgeon who has done maximum work in the field of anal fistulas across the globe, has more than 150 international research papers on the subject, and has treated fistula patients from 41 countries who were not getting cured of their dreaded fistulas in their respective countries, has maximum innovations in the field of anal fistula and has been ranked number one fistula expert by the famous US agency, Expertscape(https://www.expertscape.com/ex/rectal+fistula/c/asi)
Q. What should I do if I have a simple fistula?
If you have a simple fistula, the stakes are less than a complex fistula but still, try to get it operated by a fistula specialist because if a simple fistula is not appropriately managed, then it can become complex. As discussed, treating a complex fistula is a challenging task.
Q. What is anal fistula?
Anal fistula is a disease in which there is abnormal communication (connection/tract/ tube) between the anus or rectum and the skin in the buttocks or around the anus. The opening of the tract/tube inside the anus is known as internal opening, and the opening of the tract/tube in the skin around the anus is known as external opening. The main symptom of anal fistula is pus discharge from an opening in the skin around the anus (known as external opening).
Q. What is anal abscess? How is it different from anal fistula?
When the external opening in the skin around the anus gets blocked temporarily due to some reason, the pus accumulates in the fistula tract (tube). This acute collection is called abscess. The abscess expectedly causes swelling and moderate to severe pain. It can also cause fever and, if untreated, can cause septicemia (spread of infection in the blood to the whole body), shock (severe drop in blood pressure), and even death. An abscess is a medical emergency and should be immediately treated by an expert surgeon.
Q. What is the treatment for an Anal abscess? Can abscess and fistula be treated in a single operation?
An anal abscess is an emergency and needs urgent drainage of pus from the abscess. The drainage occurs spontaneously without any surgery if the abscess ruptures in the perianal skin. However, if the abscess doesn’t rupture spontaneously, it has to be drained surgically, and all pus should be evacuated. This is known as the incision and drainage (I & D) procedure. The fistula, if it forms, after drainage of the abscess, would require surgical treatment at a later date.
The standard accepted teaching is that an abscess needs to be drained first (spontaneously or surgically), and the fistula is operated upon later. However, now Dr. Garg has developed procedures and protocolsin which the abscess and the fistula can be treated in the first operation only in most cases. There would be no requirement for subsequent surgery.1-3 This is a big step forward as this prevents second surgery in so many patients with acute abscesses.
References
- Garg P, Kaur B. Definitive Surgery on Initial Presentation for Anal Fistula Associated With Acute Anorectal Abscess: A Definite Way Forward. Dis Colon Rectum 2022; 65(1): e 23-24 ( Click here for PubMed, Click here for DOI )
- Garg P, Kaur B, Goyal A, Yagnik VD, Dawka S, Menon GR. Lessons learned from an audit of 1250 anal fistula patients operated at a single center: A retrospective review. World J Gastrointest Surg 2021; 13(4): 340-354 ( Click here for PubMed, Click here for DOI )
- Garg P, Kaur B, Menon GR. Transanal opening of the intersphincteric space: a novel sphincter-sparing procedure to treat 325 high complex anal fistulas with long-term follow-up. Colorectal Dis 2021; 23(5): 1213-1224 ( Click here for PubMed, Click here for DOI )
Q. What are the symptoms of anal fistula?
The main symptom of anal fistula is pus discharge from an opening in the skin around the anus (external opening). The pus discharge may vary from person to person and from fistula to fistula. The discharge from the fistula may happen once a year or once a month/ week, or many times in a day. The frequency of pus discharge may have no correlation with the complexity of the fistula. A simple fistula may lead to copious discharge, while a complex fistula may lead to a bit of pus discharge, but usually, the amount of discharge correlates with the fistula complexity.
The other less common symptom of fistula is pain and swelling around the anal region. This usually happens when pus stops coming out of the external opening and causes abscess formation. This becomes a medical emergency and should be urgently treated.
If pus keeps draining outside, then fistula is usually not associated with much pain. The lack of pain does not decrease the risks and danger associated with the fistula.
In long-standing cases, there is a risk of cancer formation in the fistula tract, which is generally a more dreaded kind of cancer variety (mucinous adenocarcinoma).
Q. How is anal fistula diagnosed?
Anal fistula is mostly diagnosed on symptoms and a general examination by the doctor. The recurring symptom of pus discharge from a skin opening around the anus usually happens only in an anal fistula. On examination, the doctor can feel the fistula tract (communicating tube) from the external opening in the skin up to the anus. On gentle per rectal examination (insertion of a finger inside the anus), an experienced surgeon can also feel the internal opening of the fistula inside the anus.
The confirmation of anal fistula is done by MRI, Ultrasound (Transrectal or perineal), or X-ray Fistulogram.
Q. What are the radiological tests done for anal fistula? How do they help?
The three main radiology tests are MRI (Magnetic Resonance Imaging), Ultrasound (Transrectal or perineal), or X-ray Fistulogram. These tests help to confirm the presence ofa fistula.
MRI-Fistulogram: This is the gold-standard test for anal fistulas. It gives a lot of information about the fistula, which is not possible to know just by physical examination.
- Confirms fistula: MRI can confirm fistula where its presence is doubtful, especially when the fistula is small or causes minimal symptoms.
- Location of internal opening: MRI shows the location of the internal opening of the fistula, the closure of which is pivotal for the successful cure of fistula.
- Number of fistula branches: MRI shows the number of fistula branches (secondary tracts). This is important because even if one branch is left untreated, the fistula may recur again.
- Amount/extent and exact location of sphincter muscle involvement: MRI shows the extent and exact location of the sphincter muscle (the muscle which helps control the bowel motion) the fistula involves. This information is essential because if the surgeon is not sure about the extent and location of the sphincter muscle involved by the fistula, the surgeon may end up cutting or damaging the sphincter muscle. This can cause incontinence (loss of control over bowel motions), which is a very serious complication.
- Depth of fistula: This is important information given by MRI as, in most cases, assessing the depth of the fistula may not be possible on clinical examination
Therefore, MRI gives immense information about anal fistulas. The advent of MRI has led to a steep rise in the successful treatment of anal fistulas. It is imperative for the treating surgeons to read and interpret MRIs themselves and not to operate only by reading the radiologist’s MRI report. The reason for this is that a lot of information is lost when the information of a 3-dimensional fistula image in the mind of the radiologist is written on a piece of paper (MRI report), and then the 3-dimensional fistula image is reconstructed by the operating surgeon by reading the MRI report. It is far better if the operating surgeon reads the MRI CD or films himself and forms a 3-dimensional fistula image directly in his mind. After all, the surgery has to be done by the operating surgeon. Therefore, it is pertinent that the 3-dimensional fistula image in the surgeon’s mind is as accurate as possible. Any discrepancy in the accuracy of a 3-dimensional fistula image in the surgeon’s mind can lead to fistula recurrence.
MRI Contrast: Contrast is the medicine given by intravenous injection (by injecting medication into the patient’s vein) while the MRI is being done. The contrast medicine looks bright on MRI. Therefore, contrast medicine goes through the blood into the anal region and brightens the area with more blood supply. This makes the identification of certain types of tissues much easier. But, as per Dr. Pankaj Garg, the world authority on MRI fistulas, contrast is not needed in most cases. A good quality MRI without contrast gives all the information required to properly diagnose and manage all types of anal fistulas, and contrast is needed in very rare cases.
Ultrasound: An ultrasound gives all the information that MRI provides, but many studies have shown that ultrasound is slightly inferior to MRI. Ultrasound is of two types: transrectal (an ultrasound probe inserted inside the anus and, therefore, is a bit uncomfortable) and transperineal (an ultrasound probe is kept outside on the perineal skin and not inserted inside the anus).
The main drawback of ultrasound is that it is operator-dependent (the information gained from ultrasound solely depends on the doctor doing it). The ultrasound films or CDshave practically no use to any other doctor or the operating surgeons as they cannot extract much information from the films. This is in sharp contrast to MRI, in which the operating surgeon can extract equal (100%) information from the CD or films as the reporting radiologist. Therefore, MRI is far more valuable than ultrasound because once you have a CD of the MRI, you can go to any fistula expert surgeon, and MRI won’t be repeated. The fistula expert can gain all the vital information from the CD. It is pertinent to mention that MRI CD is far better than MRI films because in CD, unlike MRI printed films, each image is full size (of the computer screen), and no image is missed. Therefore, most fistula experts operate only after studying MRI CD in detail.
X-ray Fistulogram: In this, a dye that looks bright on the X-ray is injected into the fistula through the external opening around the anus while the X-ray is being done. The X-ray would show the coming of dye inside the anus and would thus confirm the presence of the internal opening. This is acrude test as it hardly gives any useful information. The tissues, especially the sphincter muscles, are not seen at all. This test was primarily done more than three decades back when no MRI or Ultrasound was available. But now, with the availability of MRI or Ultrasound, X-ray Fistulogram is an obsolete test and should not be done.
Q. What is the level of expertise of Dr. Pankaj Garg in the MRI-Anal fistula? What are the contributions of Dr. Pankaj Gag in the field of MRI-Anal fistula at the global level?
Dr. Garg is the leading expert in the field of MRI of anal fistulas. He has published the largest series of MRIs in anal fistula in the world.1-3
He has made guidelines for the radiologists on the interpretation of MRI after anal fistula surgery.4 He has several discoveries in MRI-anal fistula to his name which include a new anatomical space where fistula spreads, new types of the anal fistula, new parameters to be reported in MRI etc. All these have been published in top radiology journals of the USA.5,6,7,8He has also published a new eponymous scoring system – the Garg Scoring system- which accurately predicts long-term fistula healing.9This research of Dr. Garg was selected for Podium presentation in Best Paper in the annual conference of the American Society of Colon and Rectal Surgeons (ASCRS) in 2022 held at Tampa, Florida, USA .10
References
- Garg P. Comparison of Preoperative and Postoperative MRI After Fistula-in-Ano Surgery: Lessons Learnt from An Audit of 1323 MRI At a Single Centre. World J Surg 2019; 43(6): 1612-1622 ( Click here for PubMed, Click here for DOI )
- Garg P, Singh P, Kaur B. Magnetic Resonance Imaging (MRI): Operative Findings Correlation in 229 Fistula-in-Ano Patients. World J Surg 2017; 41(6): 1618-1624 ( Click here for PubMed, Click here for DOI )
- Garg P, Dawka S, Kaur B, Yagnik VD. Conservative (non-surgical) management of cryptoglandular anal fistulas: is it possible? A new insight and direction. ANZ J Surg 2022; 92(5): 1284-1285 ( Click here for PubMed, Click here for DOI )
- Garg P, Kaur B, Yagnik VD, Dawka S, Menon GR. Guidelines on postoperative magnetic resonance imaging in patients operated for cryptoglandular anal fistula: Experience from 2404 scans. World J Gastroenterol 2021; 27(33): 5460-5473 ( Click here for PubMed, Click here for NCBI, Click here for DOI )
- Garg P, Kaur B, Yagnik VD, Dawka S. A New Anatomical Pathway of Spread of Pus/Sepsis in Anal Fistulas Discovered on MRI and Its Clinical Implications. Clin Exp Gastroenterol 2021; 14: 397-404 Click here for PubMed, Click here for NCBI, Click here for DOI
- Garg P, Kaur B. The new pathways of spread of anal fistula and the pivotal role of MRI in discovering them. Abdom Radiol (NY) 2021; 46(8): 3810-3814 ( Click here for PubMed, Click here for DOI )
- Garg P, Dawka S, Yagnik VD, Kaur B, Menon GR. Anal fistula at roof of ischiorectal fossa inside levator-ani muscle (RIFIL): a new highly complex anal fistula diagnosed on MRI. Abdom Radiol (NY) 2021; 46(12): 5550-5563 ( Click here for PubMed, Click here for DOI )
- Garg P, Kaur B, Yagnik V, Dawka S. Including video and novel parameter-height of penetration of external anal sphincter-in magnetic resonance imaging reporting of anal fistula. World J Gastrointest Surg 2022; 14(4): 271-275 ( Click here for PubMed, Click here for DOI )
- Garg P, Yagnik VD, Dawka S, Kaur B, Menon GR. A Novel MRI and Clinical-Based Scoring System to Assess Post-Surgery Healing and to Predict Long-Term Healing in Cryptoglandular Anal Fistulas. Clin Exp Gastroenterol 2022; 15: 27-40 ( Click here for PubMed, Click here for NCBI, Click here for DOI )
- Garg P, Jain E. New MRI-based Scoring System to Predict Long-term Healing in Cryptoglandular Anal Fistulas. Proceedings of the Podium presentation in the BEST Paper category at American Society of Colon and Rectal Surgeons (ASCRS) annual meeting; 2022, May 1; Tampa, FL, USA.
Q. How is anal fistula treated?
The treatment of anal fistula is primarily surgery. As fistula is an abnormal physical connection between the anus/rectum and the external skin, it cannot be cured with medicines. Though medicines like antibiotics can reduce the symptoms (pus discharge) of fistula, at the most, the relief is temporary. Moreover, antibiotics cannot and should not be taken for long periods as they can cause side effects and there is a danger of developing resistance to antibiotics by the infecting bacteria. If this happens, then these antibiotics will become ineffective against those bacteria in the future.
A lot of patients ask us the question of whether in the alternate system of medicines like homeopathy and Ayurveda, there are medicines that can cure anal fistula without surgery. After successfully treating thousands of anal fistula patients from all across the world, we can confidently say that there are no medicines that can cure fistula in any medical system. Like there are antibioticsin the Allopathy (modern) system of medicine, similarly, there are antibiotic medicines in Homeopathy, Yunani, and Ayurveda systems. Unlike allopathy, the antibiotic medicines in these systems are not commonly available due to which there is far less abuse and hence much less resistance to the antibiotic medicines of these systems. Therefore, the antibiotics of these systems (Homeopathy, Yunani, and Ayurveda systems) also provide temporary relief in fistula symptoms like allopathic antibiotics. But, like allopathic antibiotics, the relief lasts only for a few months and then the fistula starts spreading despite taking antibiotics. We have yet to see even a single patient of anal fistula who has been cured permanantly with medicines of these alternate systems of medicine (Homeopathy, Yunani, and Ayurveda systems) irrespective of the wild claims being made over social media and advertisements.
Nonetheless, finally, there is a ray of hope. Dr. Pankaj Garg is aggressively working to develop treatment of anal fistulas with medicines, without the need for surgery. For the first time in the world, a treatment concept is being developed by Dr. Garg which has demonstrated that a subset of anal fistulas can be treated by medicines (without surgery).
Q. Can anal fistula be treated without surgery?
Dr. Pankaj Garg is aggressively working to develop treatment of anal fistulas with medicines, without the need for surgery. For the first time in the world, a treatment concept has been developed by Dr. Garg which has demonstrated that a subset of anal fistulas can be treated by medicines (without surgery).1 However, only a few fistula patients can be treated without surgery and a careful detailed assessment is done to decide whether the person fits in this category or not. Nonetheless, it is a big step forward that the non-surgical treatment of anal fistulas (with medicines only) has been started due to research innovations of Dr. Pankaj Garg.
References
- Garg P, Dawka S, Kaur B, Yagnik VD. Conservative (non-surgical) management of cryptoglandular anal fistulas: is it possible? A new insight and direction. ANZ J Surg 2022; 92(5): 1284-1285 ( Click here for PubMed, Click here for DOI )
Q How is Anal Fistula caused?
Most fistulas begin as anorectal abscesses. When the abscess opens or ruptures spontaneously into the anal canal (or has been opened surgically), a fistula may occur. Approximately, 8-50% of perianal abscess patients end up having an anal fistula.
Other causes of fistulas include tuberculosis, cancer, injury (trauma), Crohn’s disease, Radiation therapy, anal Fissure, and infections (actinomycoses, chlamydial, etc). Fistulas may occur singly or in multiples.
Q What are the types of Anal Fistulas?
There are broadly 4 types of anal fistulas:
Intersphincteric- Fistula tract passes between the two sphincters- 64%
Trans-sphincteric- Fistula tract crosses the two sphincters- 30%
Submusoal- Fistula tract passes between the sphincters and the mucosa of the anus and rectum 5%
Extrasphincteric- Fistula tract goes beyond the sphincter- 1%
For practical purposes, Anal Fistulas are 2 types- Low & High. Low Fistulas are present in the lower part and do not extend up to the anorectal sling [ muscle layer responsible for continence (control on the passage of motions)]. High fistulas extend up to or beyond the anorectal sling. Knowing the type of fistula is important because high fistula if not managed properly can be associated with incontinence.[loss of control on the passage of motions]
Q. Dr. Pankaj Garg has an exceptionally high cure rate for anal fistulas. What are the reasons for this?
There are several reasons for the high cure rate for anal fistulas, even complex fistulas, by Dr. Garg.
- Innovations: Dr. Garg is doing extensive research in this field for more than 15 years. Due to his diligence, hard work, his decision to focus on only one field (anal fistulas), and out of box thinking, he has innovated several new pathbreaking treatment procedures and concepts in this field. The best part of DR Garg’s innovations is that they are simple, effective, and make surgery much less painful and minimally invasive (much smaller or no cuts/ incisions). The TROPIS procedure innovated by Dr. Garg is one such minimally invasive treatment for high complex fistulas and has been shown to be the most effective sphincter-sparing procedure for complex fistulas across the globe.1 Garg classification innovated by Dr. Garg has become a favorite amongst fistula surgeons all across the world as it is far more helpful, and logical and provides treatment guidance to the operating surgeon.2 Similarly, the Garg protocol invented by Dr. Garg has shown the path to the surgeons as to how to manage the fistulas in which the internal opening is not easily locatable.3 Before the Garg protocol, there were no papers or guidelines as to how to manage such fistulas which have the highest risk of recurrence. Dr. Garg has also devised, the Garg scoring system, which when calculated in the early postoperative period (three months after surgery) can accurately predict fistula healing in the long term.4 In fact, Dr. Garg has done maximum innovations in the field of anal fistula.
- Expertise in MRI:Apart from several pathbreaking innovations, Dr. Garg is the world authority in MRI of Anal Fistulas. The details can be seen here (Link to question in this document- What is the level of expertise of Dr. Pankaj Garg in the MRI-Anal fistula? What are the contributions of Dr. Pankaj Gag in the field of MRI-Anal fistula at the global level?
- Maximum experience in anal fistulas: Patients from all over the world are referred to Dr. Garg for the expert treatment of complex and recurrent anal fistulas. Dr. Garg has successfully treated hundreds of patients from 41 countries (including the USA, UK, Canada, Australia, Europe, Africa, and middle-east) in the last five years. Dr. Garg also established the first eponymous anal fistula research institute in the world, Garg Fistula Research Institute (GFRI), at Panchkula, North India.5( Contribution of Dr. Pankaj Garg )
- Meticulous follow-up: The patients at Garg Fistula Research Institute (GFRI) are followed up very meticulously, not only in the immediate postoperative period but also for years and decades after the surgery.
References
- Huang H, Ji L, Gu Y, Li Y, Xu S. Efficacy and Safety of Sphincter-Preserving Surgery in the Treatment of Complex Anal Fistula: A Network Meta-Analysis. Front Surg 2022; 9: 825166 ( Click here for PubMed, Click here for NCBI, Click here for DOI )
- Garg P. Garg Classification for Anal Fistulas: Is It Better than Existing Classifications?—a Review. Indian Journal of Surgery 2018; 80(6): 606-608 ( Click here for DOI )
- Garg P, Kaur B, Singla K, Menon GR, Yagnik VD. A Simple Protocol to Effectively Manage Anal Fistulas with No Obvious Internal Opening. Clin Exp Gastroenterol 2021; 14: 33-44 ( Click here for PubMed, Click here for NCBI, Click here for DOI )
- Garg P, Yagnik VD, Dawka S, Kaur B, Menon GR. A Novel MRI and Clinical-Based Scoring System to Assess Post-Surgery Healing and to Predict Long-Term Healing in Cryptoglandular Anal Fistulas. Clin Exp Gastroenterol 2022; 15: 27-40 ( Click here for PubMed, Click here for NCBI, Click here for DOI )
Q. What are different procedures to treat anal fistula?
There are several procedures to treat anal fistulas. The fact that there are so many surgical procedures to treat anal fistulas clearly shows that there is no established gold-standard procedure and more active research is needed in this field than in any other field. Dr. Garg is the torchbearer and has done uthe tmost pioneering in the field of anal fistulas at the global level.
The following methods are available to treat anal fistula: –
- Fistulotomy
- Fistulectomy
- Endorectal/ Anal advancement flaps
- Seton
- Ksharsutra
- Fibrin Glue
- AFP – Anal Fistula Plug
- LIFT (Ligation of Inter-sphincteric Fistula Tract)
- VAAFT (Video-Assisted Anal Fistula Treatment)
- Laser (FiLac- Fistula laser cure)
- PERFACT
- Fixcision
- TROPIS (Transanal Opening of Intersphincteric space)
- Fistulectomy with primary sphincter repair
The two main issues with fistula treatment are incontinence (risk of losing control of motions (stools) and recurrence (fistula not getting cured or occurring again and again). These two risks become very high in complex fistulas where the recurrence rate can reach up to 50-80% if they are treated by someone who is not a renowned fistula expert. Thus, the best treatment method for fistula would cure fistula without cutting or damaging the sphincter-muscle (thus minimizing the risk of incontinence) and the recurrence rate would also be very low.
For low fistulas, fistulotomy is considered the preferred operation. Howver, for high complex fistulas, a sphincter-sparing procedure should be preferred. Amongst the several sphincter-sparing procedures available, LIFT & TROPIS have been shown to have highest cure rate.
Q How is Fistulectomy/Fistulotomy done? What are the advantages and disadvantages of this procedure?
Oldest and the best studied of all the methods. In this surgery, the fistula tract is laid open [Fistulotomy] or the fistula tract is totally taken out[Fistulectomy]. The resultant wound is generally not closed and left open to heal of its own. This way the chances of recurrence are decreased.
It is considered as one of the best options for Low Fistulas but is not recommended for High fistulas as the risk of incontinence would be high if this procedure is done in high fistulas. If the patient selection is done appropriately, then fistulotomy yields highest cure rate in anal fistulas.
Dr Garg has done maximum work and published the largest series of fistulotomy in prominent USA & European journals.1,2 He has also innovated a novel modification known as CROSS fistulotomy3 which has tremendously increased the safety and success rate of this procedure (success rate close to 99%).
References
1. Garg Pankaj. Is fistulotomy still the gold standard in present era and is it highly underutilized?: An audit of 675 operated cases. Int J Surg 2018; 56: 26-30 ( Click here for PubMed, Click here for DOI )
2. Garg Pankaj, Kaur B, Goyal A, Yagnik VD, Dawka S, Menon GR. Lessons learned from an audit of 1250 anal fistula patients operated at a single center: A retrospective review. World J Gastrointest Surg 2021; 13(4): 340-354 ( Click here for PubMed, Click here for NCBI, Click here for DOI )
3. Garg Pankaj. Standardizing the Steps of Fistulotomy to Maximize the Cure Rate and Minimize Incontinence Risk in Anal Fistula. Indian Journal of Surgery 2020; 82(6): 1325-1326 ( Click here for DOI )
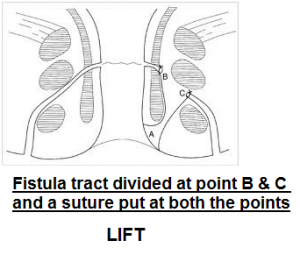
Q How is LIFT (Ligation of Intersphincteric fistula tract) ? What are the advantages and disadvantages of this procedure?
In LIFT procedure, the sphincter muscles are not divided. A cut is given and a plane is developed between the two anal sphincters and the fistula tract passing between the two sphincter muscles is isolated. This portion of fistula tract between the sphincters is ligated (tied) and excised (cut out). The internal opening of the tract is cauterized and the portion of the fistula tract outside the sphincters is curetted, cleaned and left open so that it can drain freely and get healed.
LIFT procedure has shown promising results in high fistulas and is being one of the preferred sphincter-saving procedures for complex anal fistulas. Though many studies have shown cure rate of LIFT from 75-88%, yet there are recent randomized controlled studies in which the cure rate of LIFT was between 40-50%.1One of the reasons for this is that LIFT is technically difficult and not all surgeons are able to perform it with same level of proficiency.2,3
 Another reason could be that in presence of infection (as in case of anal fistula), healing by secondary intention (by keeping the wound open) is better and preferred over healing by primary intention (closing or suturing the wound). In LIFT procedure, after ligating the fistula tract between two sphincters, the wound is allowed to appose together which is akin to healing by primary intention.
Another reason could be that in presence of infection (as in case of anal fistula), healing by secondary intention (by keeping the wound open) is better and preferred over healing by primary intention (closing or suturing the wound). In LIFT procedure, after ligating the fistula tract between two sphincters, the wound is allowed to appose together which is akin to healing by primary intention.
Due to these reasons, the TROPIS (Transanal opening of intersphincteric space) has been shown to have better cure rates than LIFT procedure.2,3
References
- Jayne DG, Scholefield J, Tolan D, Gray R, Senapati A, Hulme CT, Sutton AJ, Handley K, Hewitt CA, Kaur M, Magill L, Group FTC. A Multicenter Randomized Controlled Trial Comparing Safety, Efficacy, and Cost-effectiveness of the Surgisis Anal Fistula Plug Versus Surgeon’s Preference for Transsphincteric Fistula-in-Ano: The FIAT Trial. Ann Surg 2021; 273(3): 433-441 ( Click here for PubMed, Click here for DOI )
- Huang H, Ji L, Gu Y, Li Y, Xu S. Efficacy and Safety of Sphincter-Preserving Surgery in the Treatment of Complex Anal Fistula: A Network Meta-Analysis. Front Surg 2022; 9: 825166 ( Click here for PubMed, Click here for NCBI, Click here for DOI )
- Garg Pankaj. Comparison between recent sphincter-sparing procedures for complex anal fistulas-ligation of intersphincteric tract vs transanal opening of intersphincteric space. World J Gastrointest Surg 2022; 14(5):374-382 ( Click here for PubMed, Click here for DOI )
Q: What is TROPIS (Transanal opening of intersphincteric space) procedure?
In TROPIS procedure, the fistula tract in the intersphincteric space in laid open into the anal canal. The resulting wound is not closed and is allowed to heal by secondary intention. Due to this, healing and cure rate of TROPIS is above 90% and has been shown to be the best of all the surgical procedures available in high complex fistulas.1
TROPIS procedure was invented by Dr Pankaj Garg in 2015 and was first published in 2017 in a topmost UK journal, InternationalJournal of Surgery.2Subsequently, the high cure rate of TROPIS has been corroborated in hundreds of patients with complex anal fistula by Dr Garg and several other surgical centres across the world.3-6
In TROPIS, the healing is allowed to occur by secondary intention due to which it has been shown to have highest cure rate in complex high fistulas (better than LIFT procedure).1,7
References
- Huang H, Ji L, Gu Y, Li Y, Xu S. Efficacy and Safety of Sphincter-Preserving Surgery in the Treatment of Complex Anal Fistula: A Network Meta-Analysis. Front Surg 2022; 9: 825166 ( Click here for PubMed, Click here for NCBI, Click here for DOI )
- Garg P. Transanal opening of intersphincteric space (TROPIS) – A new procedure to treat high complex anal fistula. Int J Surg 2017; 40: 130-134 ( Click here for PubMed, Click here for DOI )
- Garg P, Kaur B, Menon GR. Transanal opening of the intersphincteric space: a novel sphincter-sparing procedure to treat 325 high complex anal fistulas with long-term follow-up. Colorectal Dis 2021; 23(5): 1213-1224 ( Click here for PubMed, Click here for DOI )
- Garg Pankaj, Kaur B, Goyal A, Yagnik VD, Dawka S, Menon GR. Lessons learned from an audit of 1250 anal fistula patients operated at a single center: A retrospective review. World J GastrointestSurg2021; 13(4): 340-354 ( Click here for PubMed, Click here for NCBI, Click here for DOI )
- Li YB, Chen JH, Wang MD, Fu J, Zhou BC, Li DG, Zeng HQ, Pang LM. Transanal Opening of Intersphincteric Space for Fistula-in-Ano. Am Surg 2021: 3134821989048 ( Click here for PubMed, Click here for DOI )
- Huang B, Wang X, Zhou D, Chen S, Li B, Wang Y, Tai J. Treating highly complex anal fistula with a new method of combined intraoperative endoanal ultrasonography (IOEAUS) and transanal opening of intersphincteric space (TROPIS). Videosurgery Miniinv 2021; 16(1): 697-703 ( Click here for DOI )
- Garg Pankaj. Comparison between recent sphincter-sparing procedures for complex anal fistulas-ligation of intersphincteric tract vs transanal opening of intersphincteric space. World J Gastrointest Surg 2022; 14(5):374-382 ( Click here for PubMed, Click here for DOI )
Q: What is LASER procedure for anal fistulas? What is the cure rate of LASER procedure in complex anal fistulas?
Laser is a focussed beam of light which is more precise in cutting and coagulating tissues. It has been in use in anal fistulas for about last 10 years. It was developed as a sphincter-sparing (sphincter-saving) procedure for complex anal fistulas. However, in most of the studies published, laser has been performed in simple fistula. The latest meta-analysis (summary of all published studies) has shown the cure rate of laser procedure between 60-70%.1 But, unfortunately, most of the patients in these studies had simple fistulas and in complex fistulas, the cure rate is expected to be lower. The reason is that the LASER procedure concentrates on burning/coagulating the external fistula tracts with laser fiber but but nothing is done effectively or differently for the internal opening of the fistula in the anus (which is the root cause of the fistula).
References
- Elfeki H, Shalaby M, Emile SH, Sakr A, Mikael M, Lundby L. A systematic review and meta-analysis of the safety and efficacy of fistula laser closure. Tech Coloproctol 2020; 24(4): 265-274 ( Click here for PubMed, Click here for DOI )
Q. What is VAAFT (Video assisted anal fistula treatment) procedure?
In VAAFT, there are two phases- diagnostic phase and a treatment phase. In diagnostic phase, a video-endoscope camera system is used so that the fistula tracts can be seen on camera/TV screen. This helps in visible inspection of the fistula lining and also helps in locating branches of fistula. In treatment phase, the fistula tract lining is ‘burnt’ or destroyed with electrocoagulation under vision.

Though the usage of modern gadget and visual inspection of fistula tract looks attractive, but in practical management, all this doesn’t add much value and doesn’t increase cure rate in any way. Whatever additional information is obtained in the diagnostic phase of VAAFT, much more information can be obtained by a preoperative MRI without touching the patient (Diagnostic phase of VAAFT is also a surgical procedure and needs anesthesia).
Secondly, as with LASER, VAAFT procedure concentrates on burning/coagulating the external fistula tracts with electrocautery under vision but nothing is done effectively or differently for the internal opening of the fistula in the anus (which is the root cause of the fistula).
Due to these reasons, the cure rate of VAAFT has been 50-70% in simple fistulas1 whereas the cure rate of VAAFT in high complex fistulas is unknown. In simple fistulas, fistulotomy offers a cure rate of 97-99% with no risk of incontinence.
References
- Garg P, Singh P. Video-Assisted Anal Fistula Treatment (VAAFT) in Cryptoglandular fistula-in-ano: A systematic review and proportional meta-analysis. Int J Surg 2017; 46: 85-91 ( Click here for PubMed, Click here for DOI )
Q: Should we go for LASER or VAAFT procedure for anal fistulas as these are the latest and most trending on media?
An important point to understand in gadget-based procedures like LASER, VAAFT, etc is that these gadgets (LASER machine, VAAFT equipment) are very costly and manufacturing companies need to sell these to doctors. Therefore, a lot of media hype is created with plenty of advertisements to project that these procedures are the simplest, safest, and the best procedures available in the market. The patients get the impression that these gadgets are ‘extraordinary’ and would cure their fistula like a ‘magic’ irrespective of whether their fistula is simple or complex. The surgeons who invest heavily and buy these expensive gadgets are also likely to fall into this loop to advertise these gadgets to the public. A suffering patient, many times, is not able to able to differentiate this blatant advertising from the facts.
In this regard, the most important point to be considered and given weightage is the expertise and skill of the surgeon rather than the gadget- A monkey with a gadget is still a monkey!
An inexperienced surgeon with a laser machine can cut the sphincter muscle and cause loss of continence (control over bowel motions). Can giving Javelin of Neeraj Chopra (Olympic gold medallist in Javelin throw in 2020) to any naïve person ensure a medal in the Olympics? NO. Therefore, gadgets or instruments are important but far far more important is the expert who is handling that gadget. Anyone can buy gadgets with money but skill is earned the harder way. Naïve surgeons promote the gadget rather than their expertise. Therefore, never fall for the gadgets but always look out for the expertise of the surgeon (how much experience the surgeon has in the field of anal fistulas, what original work the surgeon has done, how many complex fistulas the surgeon has successfully treated, etc.)
Q. What is Anal Fistula Plug & how is this procedure done?
 Anal Fistula Plug is made up of submucosa of the small intestine and is a highly sophisticated absorbable materthathich is absorbed/dissolved by the body in 6-8 weeks. This plug is placed and anchored in the fistula tract by a special technique and the internal opening is closed over it. It provides the scaffold over whithech body’s collagen gets deposited and closes the fistula. The Anal Fistula Plug (AFP) has been approved for clinical use by US FDA [United States Food & Drug Administration]-
Anal Fistula Plug is made up of submucosa of the small intestine and is a highly sophisticated absorbable materthathich is absorbed/dissolved by the body in 6-8 weeks. This plug is placed and anchored in the fistula tract by a special technique and the internal opening is closed over it. It provides the scaffold over whithech body’s collagen gets deposited and closes the fistula. The Anal Fistula Plug (AFP) has been approved for clinical use by US FDA [United States Food & Drug Administration]-
Initially, a high cure rate of 75-88% was reported for anal fistula plug but over time, this has dropped to 20-50%. Dr. Pankaj Garg started the anal fistula plug procedure in Asia in 2005 and has done maximum experience with anal fistula plug in India.. Dr Garg has several publications on anal fistula plug in top international surgery journals.1-4 Now, the anal fistula plug procedure is done in carefully selected patients.
References
- Garg P, Song J, Bhatia A, Kalia H, Menon GR. The efficacy of anal fistula plug in fistula-in-ano: a systematic review. Colorectal Dis 2010; 12(10): 965-970 ( Click here for PubMed, Click here for DOI )
- Garg P. To determine the efficacy of anal fistula plug in the treatment of high fistula-in-ano: an initial experience. Colorectal Dis 2009; 11(6): 588-591 ( Click here for PubMed, Click here for DOI )
- Garg P. Flaps, Glues and Plugs- A view from the East. Semin Colon Rectal Surg 2009; 20(1): 52-57 ( Click here for DOI )
- Garg P. Acellular extracellular matrix anal fistula plug: results in high fistula-in-ano awaited. World J Gastroenterol 2008; 14(46): 7143 ( Click here for PubMed, Click here for NCBI, Click here for DOI )
Q. How is Advancement flap treatment done and what are the disadvantages of this procedure?
Advancement flap is an old method in which the internal opening is covered with a flap of anal mucosa and a layer of the sphincter muscle. This procedure is technically difficult and associated with relatively high incontinence risk and rate of recurrence. Therefore, it is not very popular in most parts of the world.
Q. What is Ksharsutra or Seton treatment?
Ksharsutra was a traditional ayurvedic treatment in which the kshar (alkali-based chemical) coated thread was loosely inserted into the fistula tract. The chemical reaction by the kshar (chemical) caused fibrosis inside the fistula tract and led to its closure. The important thing to understand is that in traditional Ksharsutra, the chemical-coated thread was inserted loosely and was put tightly. Due to this, the Ksharsutra (loose) was safe as it didn’t cut or damage the anal sphincter muscle (the muscle which controls the bowel motions). If a Ksharsutra or any thread is put tightly, then it slowly cuts through the anal sphincter muscle and damages it, which carries a high risk of incontinence (loss of control of bowel motions). Not only does it cut the anal sphincter muscle but this process is extremely painful.
The expertise of original loose Ksharsutra is rare and unfortunately, in the guise of Ksharsutra, most surgeons and ayurvedic doctors are performing tight cutting seton/ Ksharsutra procedures. This procedure (tight cutting seton/ Ksharsutra) is safe when performed in a low simple fistula as not much sphincter muscle is involved. However, if a tight cutting seton/ Ksharsutra procedure is performed in a high complex anal fistula, it can lead to a disaster. Not only it is extremely painful but it causes incontinence (loss of control over bowel motions) in so many cases. Therefore, it is mandatory to ensure that before initiating any tight cutting seton/ Ksharsutra procedure, a proper evaluation of the fistula by MRI is done to see whether the fistula is high or low. If the fistula is high and more than one-third of the anal sphincter is involved by the fistula, then the Ksharsutra or cutting seton is strictly avoided at all costs.
Q. How is Fibrin glue treatment done and what are the disadvantages of this procedure?
Fibrin glue is made from plasma protein which is used to seal up and heal the fistula tract rather than cutting it open. In this procedure, the tract is cleared after which the internal opening is stitched closed and the glue is injected through the external opening. The glue is of 2 types-Autologous or Commercially prepared fibrin sealant. However, the long-term cure rate with glue is less than 20% due to which it has become obsolete.
Q. What is the contribution of Dr. Pankaj Garg in the field of anal fistulas? Has Dr. Garg done maximum work in the field of anal fistulas and is recognized as the topmost fistula expert in the world? If yes, why?
Dr. Garg Is Ranked Number -1 In the Field of Anal Fistulas in The World
Dr. Garg is the topmost researcher as well as clinician in the field of Anal Fistulas
He has done maximum work in the field of anal fistula in the world (>60 publications) and is the undisputed number one fistula expert in the world. Anal fistula is a bad disease known for its recurrences (the disease keeps coming back again and again). In this field, Dr. Garg has the best possible success rate in the world, has done maximum innovations in the world, has the highest turnover of patients in the world, and treated patients from maximum countries. There would be very few doctors in the country who are number one in their field in the world!
The fascinating aspect is that Dr. Garg has become number one in the field of his work with zero research budget surpassing fellow experts from the USA, UK, Europe, and Australia who are better placed and equipped with several times more resources.
This figure was used by an expert recently who recommended Dr. Garg for a prestigious award

A brief about the work of Dr Garg in the field of Anal fistulas is as follows: –
- Largest series of anal fistula in medical literature (1250 patients)[1]
- Largest series of exclusive complex high fistulas with long-term follow-up (408 patients)[1, 2]
- Largest series of Supralevator fistulas with long-term follow-up (129 patients)[1, 3]
- Largest series of Preoperative and Postoperative MRI in anal fistulas (2404 MRI)[4-6]
- Largest series of Anorectal Tuberculosis (776 patients, 1336 samples)[7-9]
- Largest series of fistulotomy to treat anal fistulas (611 patients)[1, 10, 11]
- New useful Classification of Anal Fistula (Garg classification)[12-14]
- Cardinal Principles to treat Complex Anal Fistula (Garg cardinal principles)[15-17]
- New Protocol to treat Anal fistula with No obvious internal opening (Garg protocol) [18, 19]
- Guidelines to interpret MRI in postoperative period after fistula surgery[4]
- A new anatomical space where fistula spreads (Outersphincteric of Garg space)[20, 21]
- A new type of highly complex fistula (RIFIL fistulas)[22]
- A new parameter-HOPE- as a parameter in MRI reporting of anal fistulas[23]
- Innovation of TROPIS Procedure- Highly effective to treat high complex and supralevator fistulas (healing rate>90% over long-term)[2, 24]
- Innovation of Tube in tract and PERFACT procedures for anal fistula[25-27]
- Management of circumrectal fistulas (completely encircling the anorectum)[28]
- Management of additional supralevator rectal opening in supralevator fistulas[29]
- First Proportional meta-analysis on VAAFT and anal fistula plug[30, 31]
- IRIP (inability to raise intraabdominal pressure) phenomenon as a cause of urinary retention after fistula surgery[32]
- First series of Anal Fistula and Pilonidal Sinus Disease coexisting simultaneously[33]
- First paper to objectively demonstrate role of MRI to confirm long-term healing in complex high cryptoglandular anal fistulas (151 cases)[34]
- First Guidelines on postoperative MRI in patients operated for cryptoglandular anal fistula (2404 MRI)[4]
- A new scoring system to accurately predict long-term healing in cyrptoglandular fistulas[35, 36]
References
1. Garg P, Kaur B, Goyal A, Yagnik VD, Dawka S, Menon GR. Lessons learned from an audit of 1250 anal fistula patients operated at a single center: A retrospective review. World J Gastrointest Surg 2021; 13(4): 340-354 ( Click here for PubMed, Click here for DOI )
2. Garg P, Kaur B, Menon GR. Transanal opening of the intersphincteric space: a novel sphincter-sparing procedure to treat 325 high complex anal fistulas with long-term follow-up. Colorectal Dis 2021; 23(5): 1213-1224 ( Click here for PubMed, Click here for DOI )
3. Garg P. Understanding and Treating Supralevator Fistula-in-Ano: MRI Analysis of 51 Cases and a Review of Literature. Dis Colon Rectum 2018; 61(5): 612-621 ( Click here for PubMed, Click here for DOI )
4. Garg P, Kaur B, Yagnik VD, Dawka S, Menon GR. Guidelines on postoperative magnetic resonance imaging in patients operated for cryptoglandular anal fistula: Experience from 2404 scans. World J Gastroenterol 2021; 27(33): 5460-5473 [PMID: 34588745 PMCID: PMC8433608 DOI: 10.3748/wjg.v27.i33.5460] ( Click here for PubMed, Click here for DOI )
5. Garg P. Comparison of Preoperative and Postoperative MRI After Fistula-in-Ano Surgery: Lessons Learnt from An Audit of 1323 MRI At a Single Centre. World J Surg 2019; 43(6): 1612-1622 ( Click here for PubMed, Click here for DOI )
6. Garg P, Singh P, Kaur B. Magnetic Resonance Imaging (MRI): Operative Findings Correlation in 229 Fistula-in-Ano Patients. World J Surg 2017; 41(6): 1618-1624 ( Click here for PubMed, Click here for DOI )
7. Garg P, Goyal A, Yagnik VD, Dawka S, Menon GR. Diagnosis of anorectal tuberculosis by polymerase chain reaction, GeneXpert and histopathology in 1336 samples in 776 anal fistula patients. World J Gastrointest Surg 2021; 13(4): 355-365 ( Click here for PubMed, Click here for DOI )
8. Garg P, Garg M, Das BR, Khadapkar R, Menon GR. Perianal Tuberculosis: Lessons Learned in 57 Patients From 743 Samples of Histopathology and Polymerase Chain Reaction and a Systematic Review of Literature. Dis Colon Rectum 2019; 62(11): 1390-1400 ( Click here for PubMed, Click here for DOI )
9. Garg P. Comparison of histopathology and real-time polymerase chain reaction (RT-PCR) for detection of Mycobacterium tuberculosis in fistula-in-ano. Int J Colorectal Dis 2017; 32(7): 1033-1035 ( Click here for PubMed, Click here for DOI )
10. Garg P. Is fistulotomy still the gold standard in present era and is it highly underutilized?: An audit of 675 operated cases. Int J Surg 2018; 56: 26-30 ( Click here for PubMed, Click here for DOI )
11. Garg P. Standardizing the Steps of Fistulotomy to Maximize the Cure Rate and Minimize Incontinence Risk in Anal Fistula. Indian Journal of Surgery 2020; 82(6): 1325-1326 ( Click here for DOI )
12. Garg P. Assessing validity of existing fistula-in-ano classifications in a cohort of 848 operated and MRI-assessed anal fistula patients – Cohort study. Ann Med Surg (Lond) 2020; 59: 122-126 ( Click here for PubMed, Click here for DOI )
13. Garg P. Garg Classification for Anal Fistulas: Is It Better than Existing Classifications?—a Review. Indian Journal of Surgery 2018; 80(6): 606-608 ( Click here for DOI )
14. Garg P. Comparing existing classifications of fistula-in-ano in 440 operated patients: Is it time for a new classification? A Retrospective Cohort Study. Int J Surg 2017; 42: 34-40 ( Click here for PubMed, Click here for DOI )
15. Garg P. A new understanding of the principles in the management of complex anal fistula. Med Hypotheses 2019; 132: 109329 ( Click here for PubMed, Click here for DOI )
16. Garg P, Sodhi SS, Garg N. Management of Complex Cryptoglandular Anal Fistula: Challenges and Solutions. Clin Exp Gastroenterol 2020; 13: 555-567 ( Click here for PubMed, Click here for DOI )
17. Garg P. Intersphincteric Component in a Complex Fistula-in-Ano Is Like an Abscess and Should Be Treated Like One. Dis Colon Rectum 2018; 61(4): e26 ( Click here for PubMed, Click here for DOI )
18. Garg P, Kaur B, Singla K, Menon GR, Yagnik VD. A Simple Protocol to Effectively Manage Anal Fistulas with No Obvious Internal Opening. Clin Exp Gastroenterol 2021; 14: 33-44 ( Click here for PubMed, Click here for DOI )
19. Garg P, Kaur B, Yagnik VD, Dawka S, Sohal A, Menon GR. Non-locatable internal opening in anal fistula associated with acute abscess and its management. World J Gastrointest Surg 2022; Accepted, under print
20. Garg P, Kaur B. The new pathways of spread of anal fistula and the pivotal role of MRI in discovering them. Abdom Radiol (NY) 2021; 46(8): 3810-3814 ( Click here for PubMed, Click here for DOI )
21. Garg P, Kaur B, Yagnik VD, Dawka S. A New Anatomical Pathway of Spread of Pus/Sepsis in Anal Fistulas Discovered on MRI and Its Clinical Implications. Clin Exp Gastroenterol 2021; 14: 397-404 ( Click here for PubMed, Click here for DOI )
22. Garg P, Dawka S, Yagnik VD, Kaur B, Menon GR. Anal fistula at roof of ischiorectal fossa inside levator-ani muscle (RIFIL): a new highly complex anal fistula diagnosed on MRI. Abdom Radiol (NY) 2021; 46(12): 5550-5563 ( Click here for PubMed, Click here for DOI )
23. Garg P, Kaur B, Yagnik V, Dawka S. Inclusion of a video and a novel parameter-HOPE- in MRI reporting of Anal fistula. World J Gastrointest Surg 2022; (Accepted, under print)
24. Garg P. Transanal opening of intersphincteric space (TROPIS) – A new procedure to treat high complex anal fistula. Int J Surg 2017; 40: 130-134 ( Click here for PubMed, Click here for DOI )
25. Garg P. Tube in tract technique: a simple alternative to a loose draining seton in the management of complex fistula-in-ano–a video vignette. Colorectal Dis 2016; 18(1): 107 ( Click here for PubMed, Click here for DOI )
26. Garg P. PERFACT procedure to treat supralevator fistula-in-ano: A novel single stage sphincter sparing procedure. World J Gastrointest Surg 2016; 8(4): 326-334 ( Click here for PubMed, Click here for DOI )
27. Garg P, Garg M. PERFACT procedure: a new concept to treat highly complex anal fistula. World J Gastroenterol 2015; 21(13): 4020-4029 ( Click here for PubMed, Click here for DOI )
28. Garg P, Kaur B, Yagnik VD, Menon GR. Extreme horseshoe and circumanal anal fistulas-challenges in diagnosis and management. Tzu Chi Med J 2021; 33(4): 374-379 ( Click here for PubMed, Click here for DOI )
29. Garg P, G RM, Kaur B. Comparison of different methods to manage supralevator rectal opening in anal fistulas: A retrospective cohort study. Cir Esp (Engl Ed) 2021; 16: S0009-0739X(0021)00114-00117 ( Click here for PubMed, Click here for DOI )
30. Garg P, Singh P. Video-Assisted Anal Fistula Treatment (VAAFT) in Cryptoglandular fistula-in-ano: A systematic review and proportional meta-analysis. Int J Surg 2017; 46: 85-91 ( Click here for PubMed, Click here for DOI )
31. Garg P, Song J, Bhatia A, Kalia H, Menon GR. The efficacy of anal fistula plug in fistula-in-ano: a systematic review. Colorectal Dis 2010; 12(10): 965-970 ( Click here for PubMed, Click here for DOI )
32. Garg P. Inability to raise intraabdominal pressure (IRIP): a common missed cause of postoperative urinary retention after anorectal surgery. Tech Coloproctol 2020; 24(5): 499 ( Click here for PubMed, Click here for DOI )
33. Garg P. Anal fistula and pilonidal sinus disease coexisting simultaneously: An audit in a cohort of 1284 patients. Int Wound J 2019; 16(5): 1199-1205 ( Click here for PubMed, Click here for DOI )
34. Garg P, Yagnik VD, Kaur B, Menon GR, Dawka S. Role of MRI to confirm healing in complex high cryptoglandular anal fistulas: long-term follow-up of 151 cases. Colorectal Dis 2021; 23(9): 2447-2455 ( Click here for PubMed, Click here for DOI )
35. Garg P, Yagnik VD, Dawka S, Kaur B, Menon GR. A Novel MRI and Clinical-Based Scoring System to Assess Post-Surgery Healing and to Predict Long-Term Healing in Cryptoglandular Anal Fistulas. Clin Exp Gastroenterol 2022; 15: 27-40 ( Click here for PubMed, Click here for DOI )
36 Garg P, Kumar P, Sasmal P, Sachdeva M, Jain M. A novel MRI-based scoring system to assess post-surgery healing and to predict long-term healing in cryptoglandular anal fistulas. Colorectal Disease 2022; 24(S1): 32, O054 (Oral Presentation) ( Click here for DOI )
